Filter results
You can narrow down the results using the filters
Audience
Topics
Our work
Diseases
Year
117 results
-
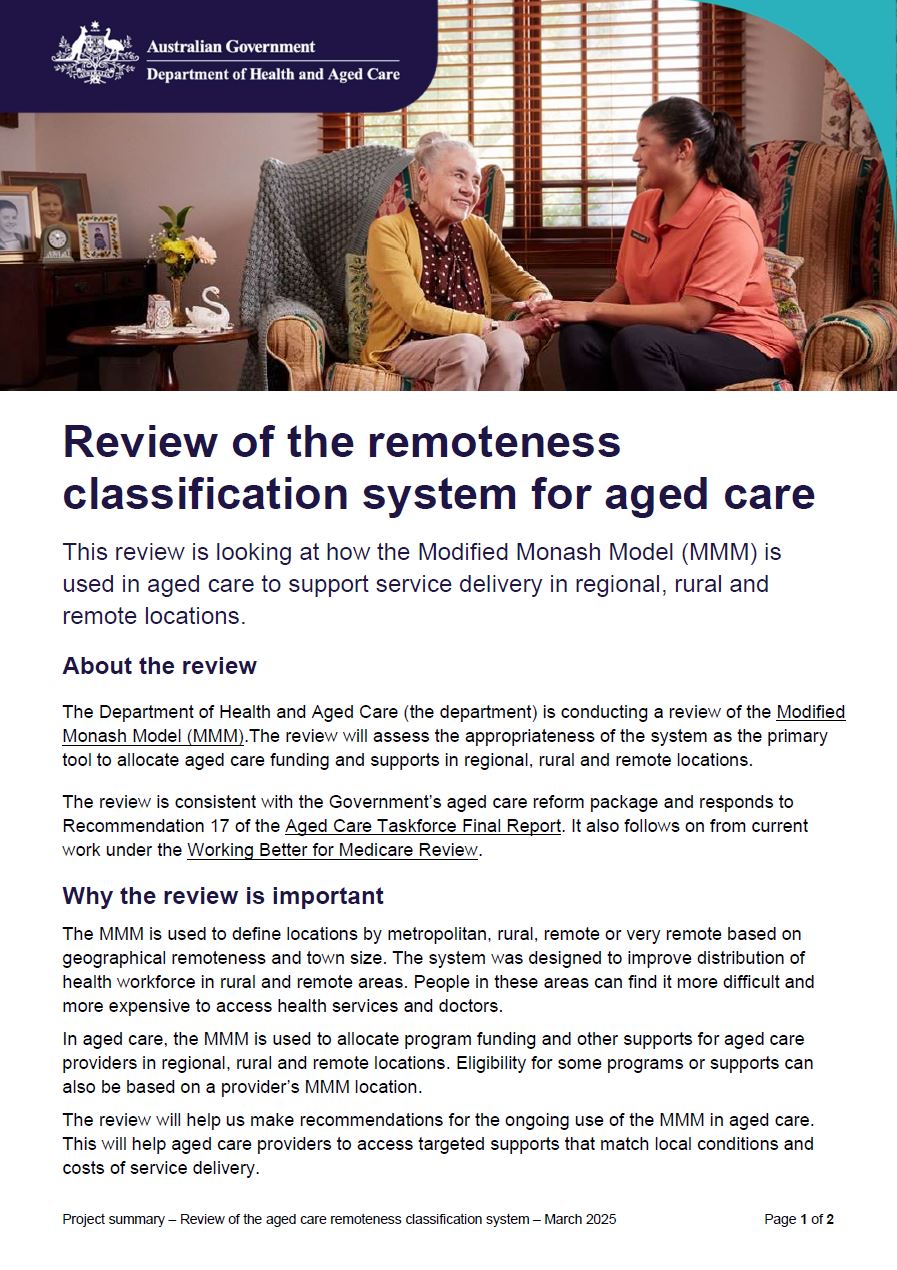
Review of the remoteness classification system for aged care – fact sheet
This fact sheet explains the review of the remoteness classification system for aged care. It looks at the use of the Modified Monash Model (MMM) in aged care to support service delivery in regional, rural and remote locations. -
Primary Health Networks (PHN) (2017) – concordance files – Australian Statistical Geography Standards (2016) – Statistical Area Level 2
Researchers can use these concordance files for Australian Statistical Geography Standards (ASGS) Statistical Area Level 1 to Primary Health Networks to undertake geospatial and data analysis. -
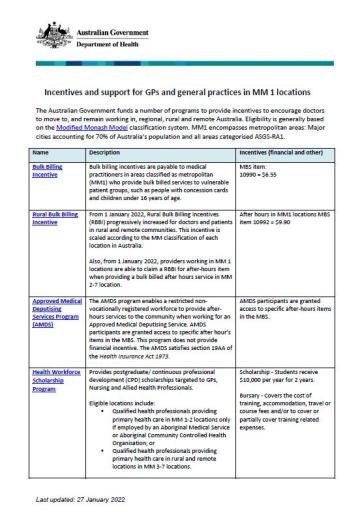
Incentives and support for GPs and general practices in MM locations
This collection contains the Modified Monash (MM) categories MM 1 to MM 7 fact sheets. -
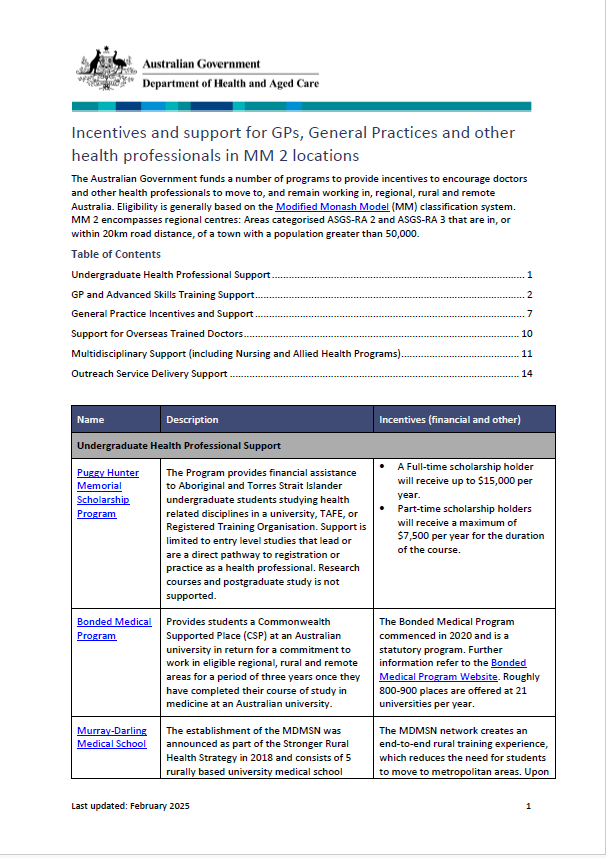
Incentives and support for GPs and general practices in Modified Monash 2 locations
The Modified Monash (MM) fact sheet for category MM 2 covers regional areas. -
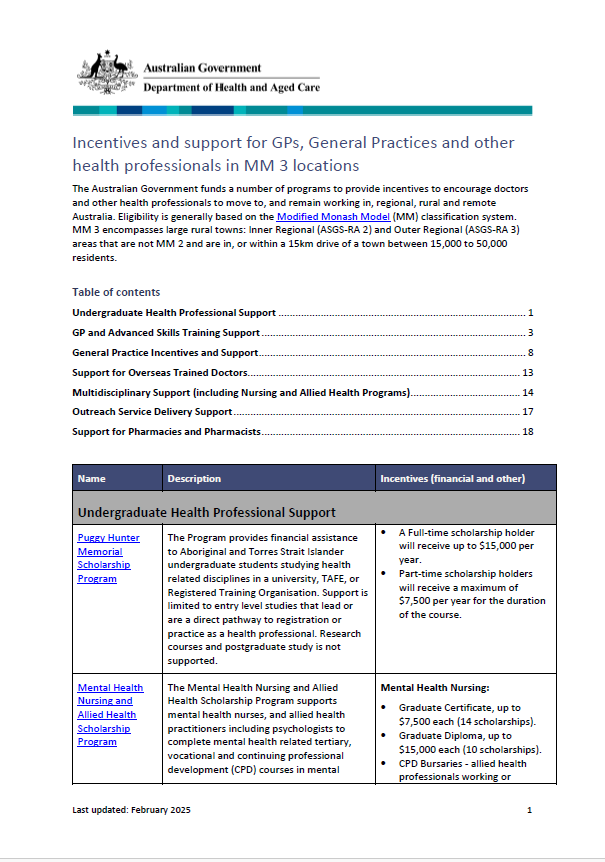
Incentives and support for GPs and general practices in Modified Monash 3 locations
The Modified Monash (MM) fact sheet for category MM 3 covers rural towns. -
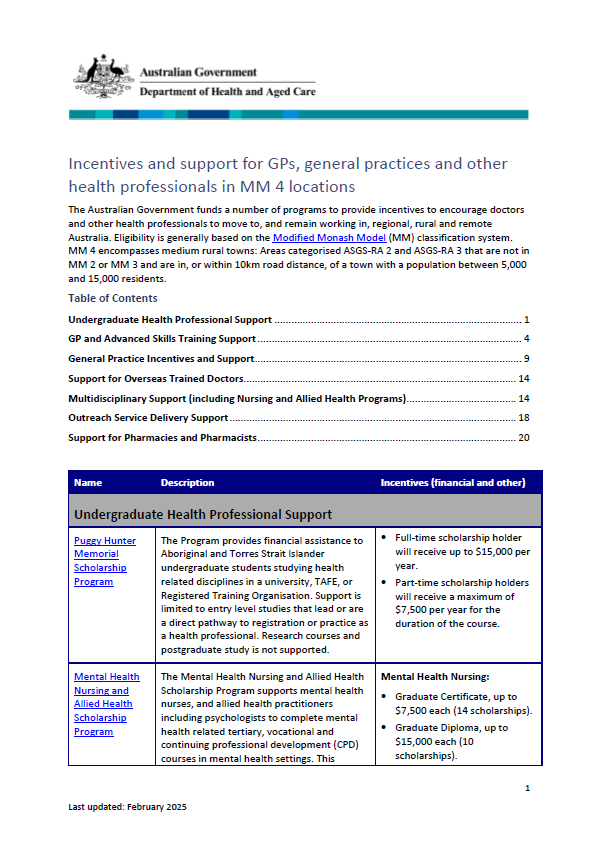
Incentives and support for GPs and general practices in Modified Monash 4 locations
The Modified Monash (MM) fact sheet for category MM 4 covers medium rural towns. -
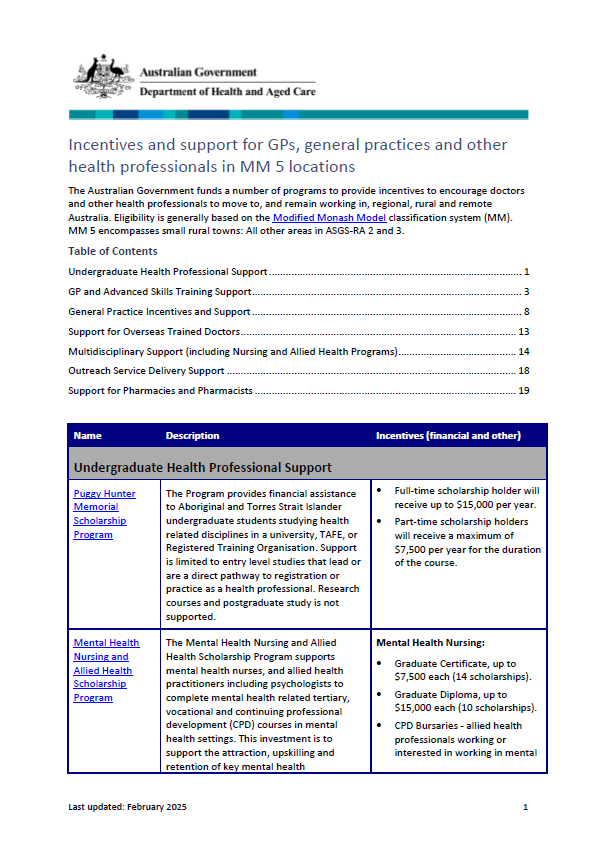
Incentives and support for GPs and general practices in Modified Monash 5 locations
The Modified Monash (MM) fact sheet for category MM 5 covers small rural towns. -
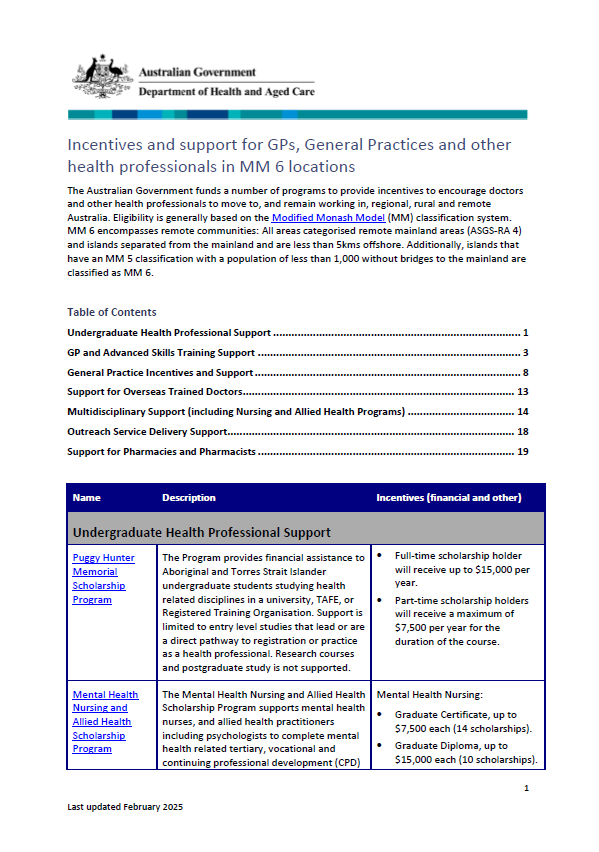
Incentives and support for GPs and general practices in Modified Monash 6 locations
The Modified Monash (MM) fact sheet for category MM 6 covers remote communities. -
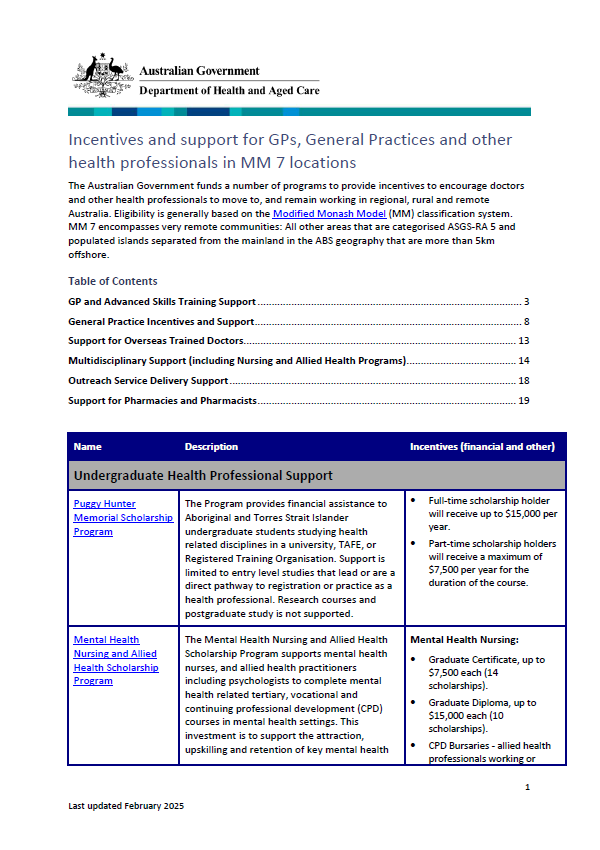
Incentives and support for GPs and general practices in Modified Monash 7 locations
The Modified Monash (MM) fact sheet for category MM 7 covers very remote communities. -
Rural Health Outreach Fund – Service Delivery Standards (SDS)
These standards provide fundholders with the information required to deliver the most efficient and effective services to address RHOF’s priorities. -
Statement of Intent from the National Rural Health Commissioner – 2 September 2024 to 30 June 2026
The Statement of Intent outlines the National Rural Health Commissioner’s priorities and approach to achieving the obligations referred to in the Assistant Minister’s Statement of Expectations. -
Office of the National Rural Health Commissioner – Annual report 2023-24
The annual report covers the commissioner’s activities from 1 July 2023 to 30 June 2024. -
Innovative Models of Care (IMOC) Program – CP@clinic
Sunraysia Community Health Services will deliver the CP@clinic under the Innovative Models of Care Program to provide community paramedic coordinated care across 4 community health services. -
Statement of Expectations for the National Rural Health Commissioner – 2 September 2024 to 30 June 2026
This statement sets out the Australian Government’s expectations for the National Rural Health Commissioner for 2 September 2024 to 30 June 2026. -
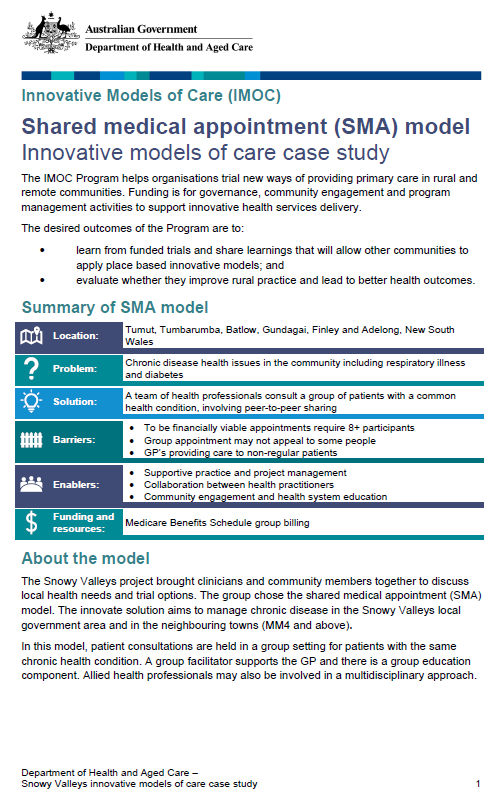
Case study – Snowy Valleys shared medical appointment model
The Snowy Valleys project is a shared medical appointment where health professionals consult patients with common health conditions, involving peer-to-peer sharing. This model included 3 separate trials, in which 2 produced sufficient billings through Medicare to satisfy participating GPs. -

Case study – Wentworth ACCHO-led sustainable GP model
An Aboriginal Medical Service opened networked primary care clinics after the local general practices closed. The model services the whole community and has outreach services to other communities. It has since attracted several GPs to Wentworth and maintained a quality primary care service. -
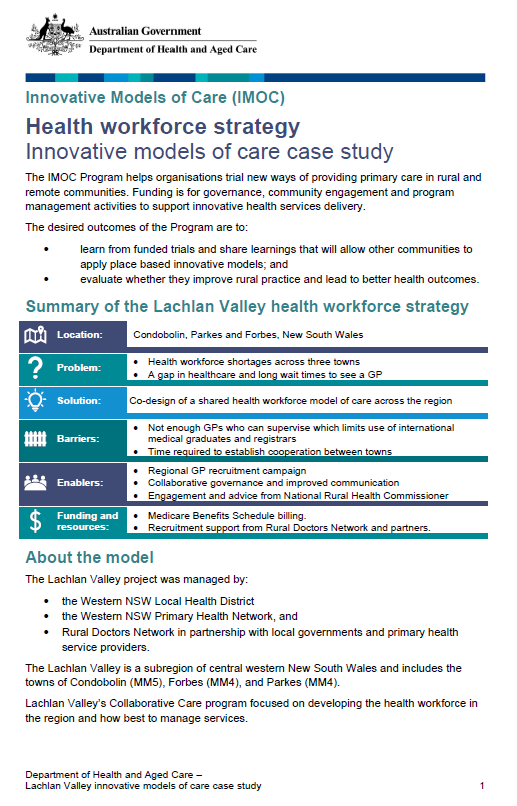
Case study – Lachlan Valley health workforce strategy
The Lachlan Valley trial aimed to test and evaluate unique models of primary care to meet community health needs in 3 rural NSW towns. No model of care was identified and trialled. However, by using a co-design process the communities identified solutions to improve access to primary health care. -
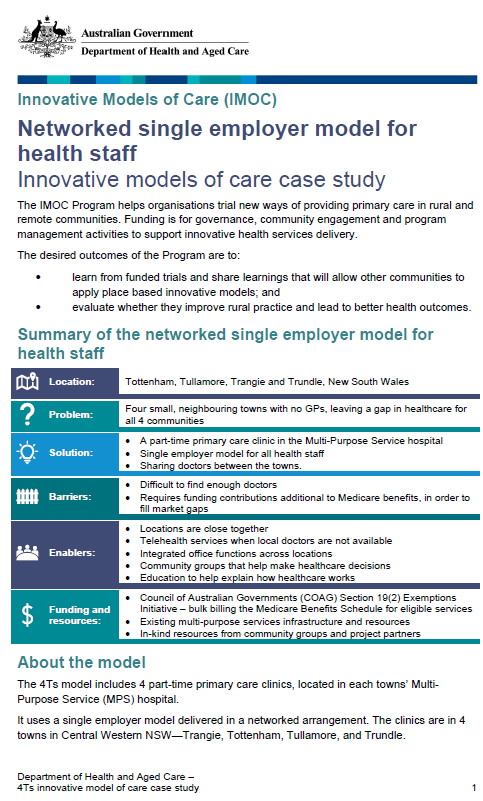
Case study – 4Ts networked single employer GP model
The towns of Trangie, Tottenham, Tullamore and Trundle have no GPs. The 4Ts model provides a single employer, and shares doctors between 4 part-time primary care clinics, located in each towns’ Multi-Purpose Service hospital. The model has decreased MPS emergency presentations and readmission rates. -
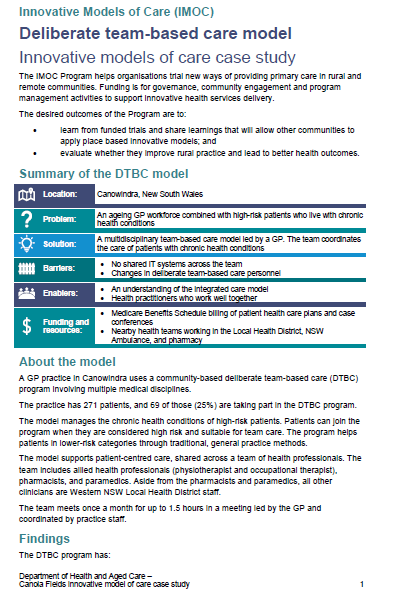
Case study – Canola Fields deliberate team-based care model
A GP practice in Canowindra uses a community-based deliberate team-based care (DTBC) program. The model supports patient-centred care, shared across a team of health professionals. The DTBC program has reduced hospitalisations, improved access to care, and reduced treatment waiting times. -
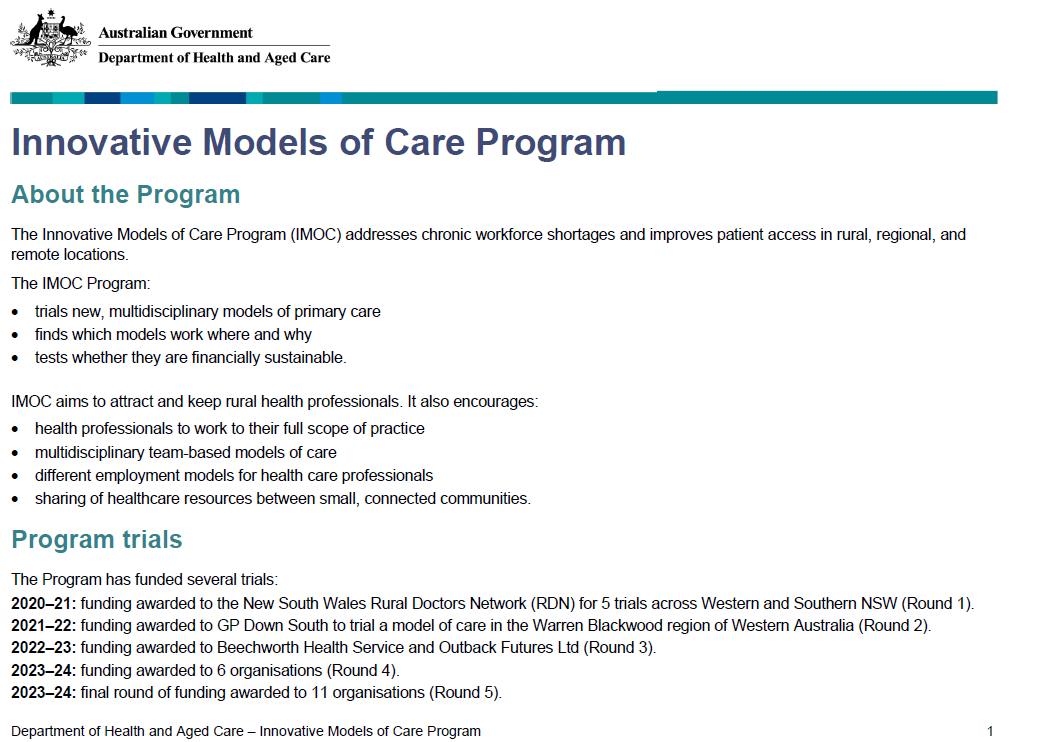
Innovative Models of Care Program
The Innovative Models of Care Program (IMOC) addresses chronic workforce shortages and improves patient access in rural, regional, and remote locations. -
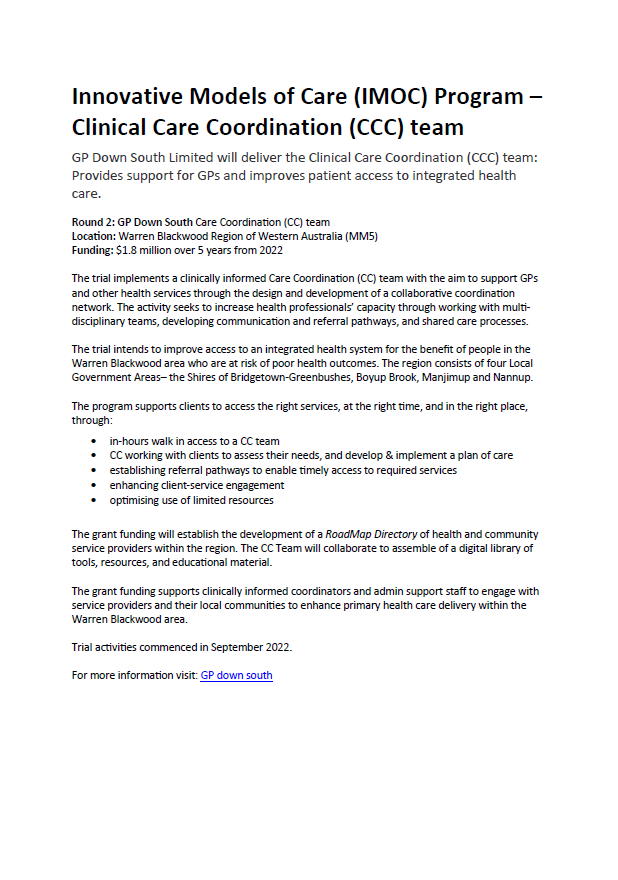
Innovative Models of Care (IMOC) Program – Clinical Care Coordination team
GP Down South Limited will deliver the Clinical Care Coordination (CCC) team under the Innovative Models of Care Program to provide support for general practitioners and improve patient access to integrated health care. -
Innovative Models of Care (IMOC) Program – Improve comprehensive care planning for older people across four multi-disciplinary areas of health care
Beechworth Health Service will deliver the Improve comprehensive care planning for older people across four multi-disciplinary areas of health care tool under the Innovative Models of Care Program: what matters, medications, mobility, and mental health (4Ms). -
Innovative Models of Care (IMOC) Program – Work-In-Work-Out (WIWO)
Outback Futures Ltd will deliver the Work-In-Work-Out (WIWO) multi-disciplinary model under the Innovative Models of Care Program to improve access to allied health professionals. -
Innovative Models of Care (IMOC) Program – Age Well Community Centre
Southern Cross Care Limited will deliver the Age Well Community Centre under the Innovative Models of Care Program to provide a range of aged care and health services. -
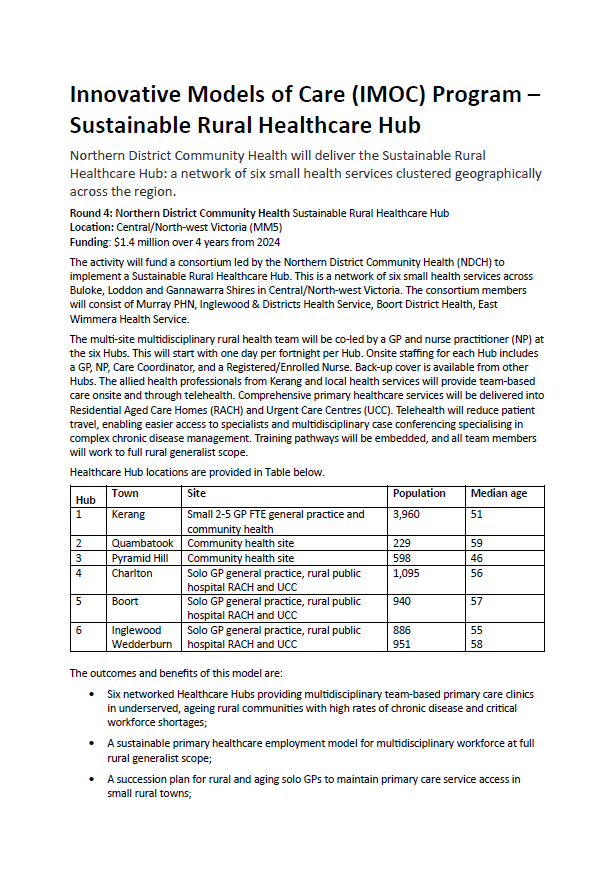
Innovative Models of Care (IMOC) Program – Sustainable Rural Healthcare Hub
Northern District Community Health will deliver the Sustainable Rural Healthcare Hub under the Innovative Models of Care Program to provide a network of 6 small health services clustered geographically across the region.