Filter results
You can narrow down the results using the filters
Audience
Topics
Our work
Year
42 results
-
Review of Medicare Integrity and Compliance
The Minister for Health and Aged Care has requested an independent, high-level review of the Integrity of Medicare and the compliance mechanisms. The review will focus primarily on the Medical Benefits Scheme. -
AskMBS Advisory #1 – General practice services
Advice for health providers and other users of the Medicare Benefits Schedule on the interpretation and application of MBS items, explanatory notes and associated legislation, to assist them in billing Medicare correctly. -
AskMBS Advisory #2 – General practice services
Advice for health providers and other users of the Medicare Benefits Schedule on the interpretation and application of MBS items, explanatory notes and associated legislation, to assist them in billing Medicare correctly. -
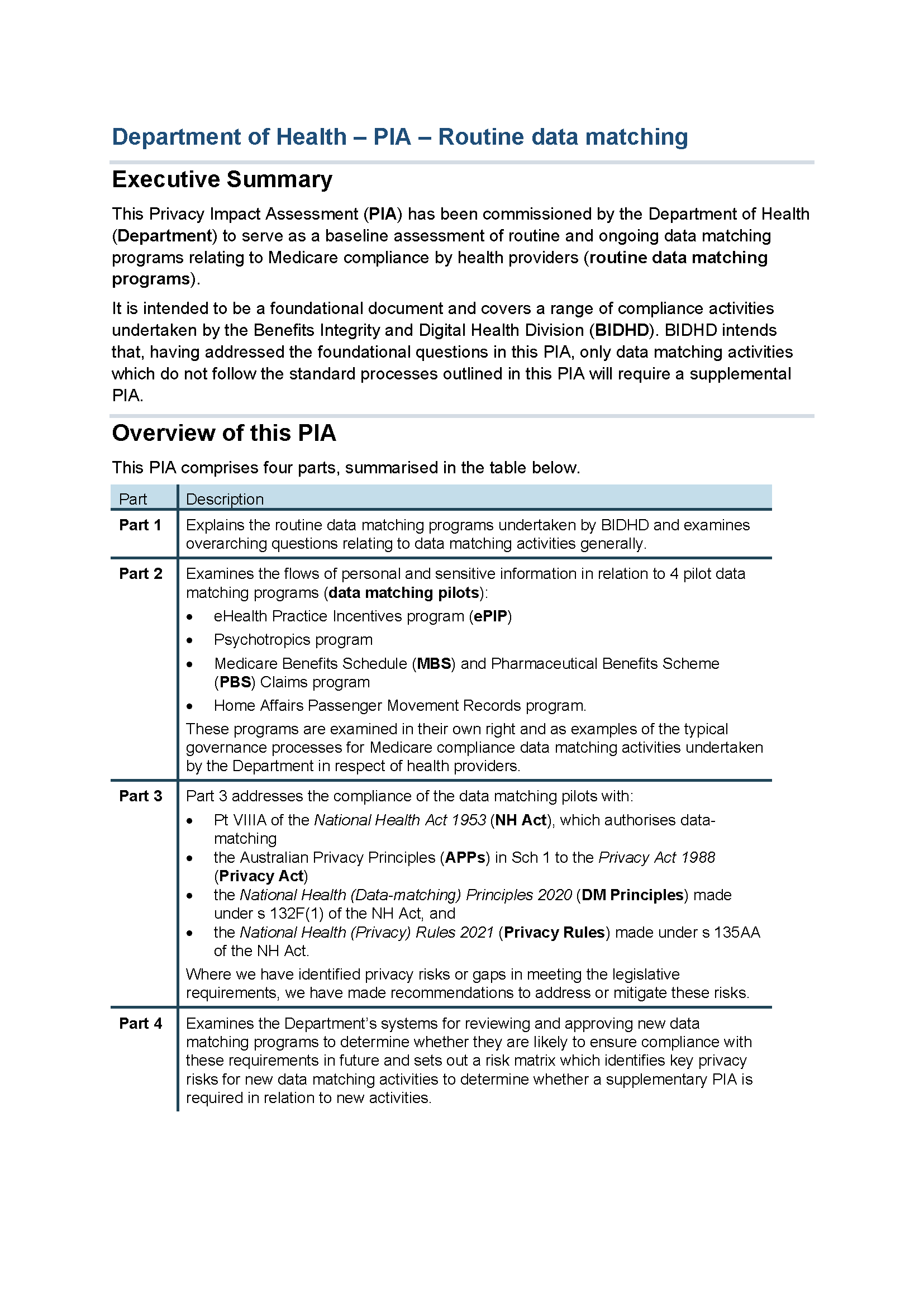
Data matching foundational – Privacy Impact Assessment – Executive summary
This Privacy Impact Assessment (PIA) executive summary serves as a baseline assessment of routine and ongoing data matching programs relating to Medicare compliance by health providers. It is intended to cover a range of compliance activities undertaken by the Department.
-
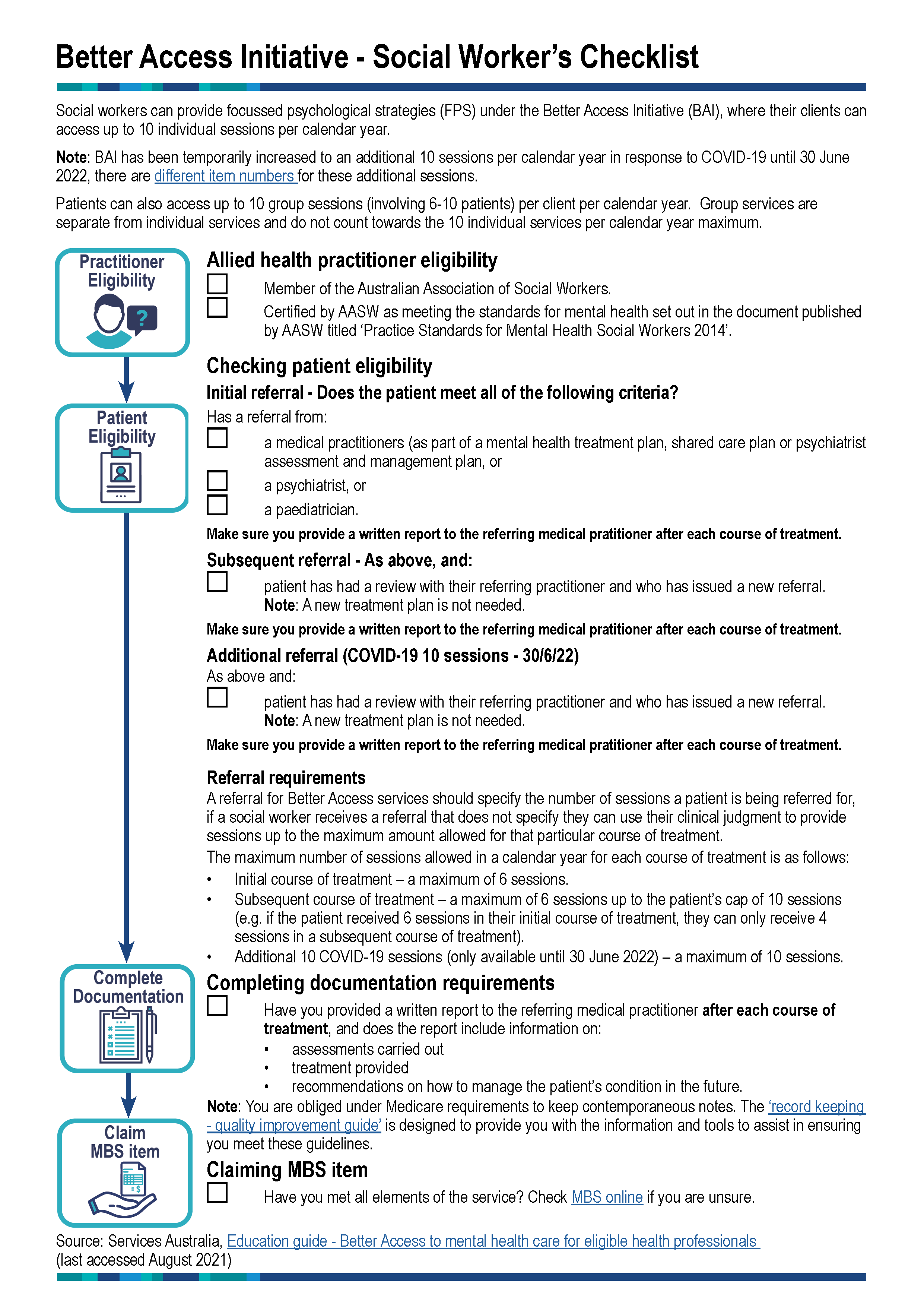
Better Access Initiative Checklist - Social Workers
Social workers can provide focussed psychological strategies (FPS) under the Better Access Initiative (BAI), where their clients can
access up to 10 individual sessions per calendar year.
-
AskMBS Advisory – Non-GP specialist and consultant physician services
Advice for health providers and other users of the Medicare Benefits Schedule on the interpretation and application of MBS items, explanatory notes and associated legislation, to assist them in billing Medicare correctly. -
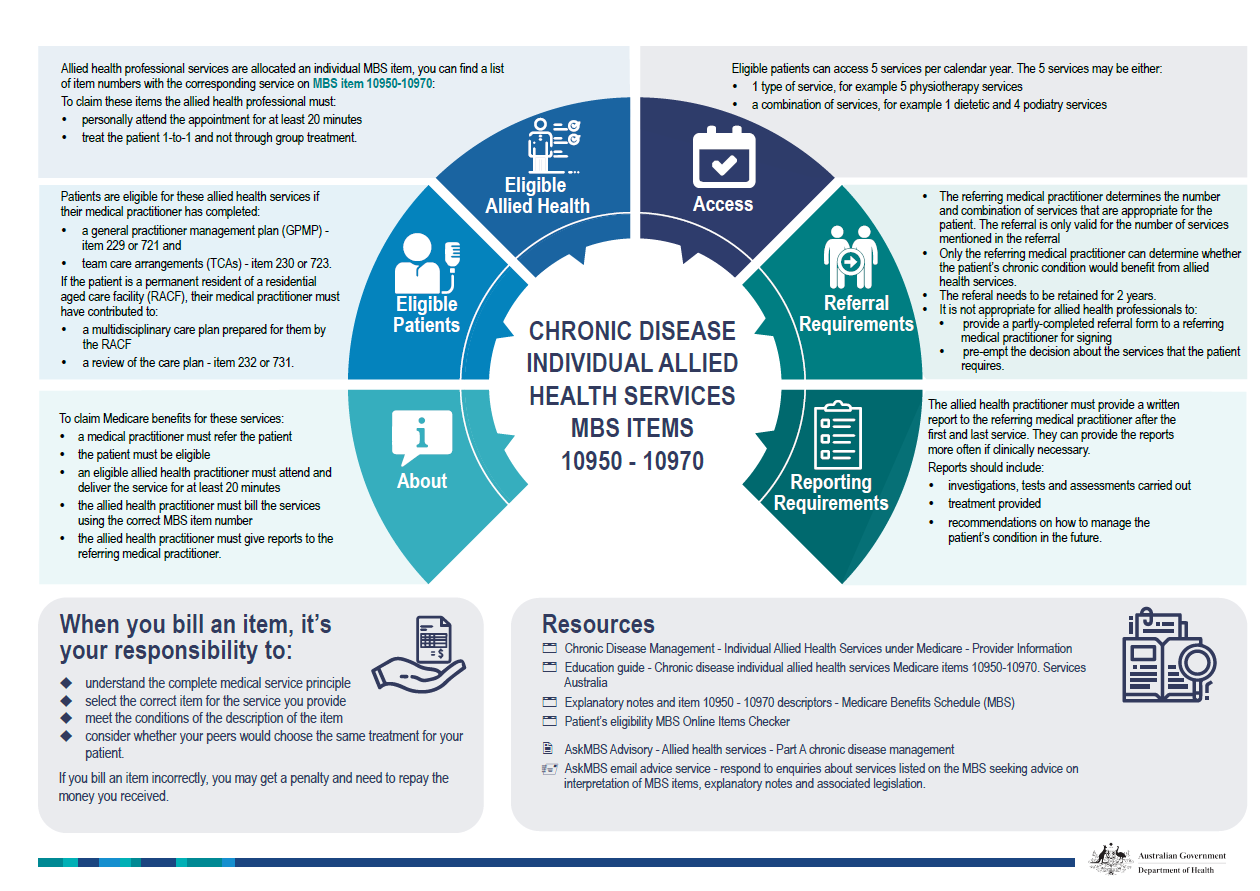
Chronic disease individual allied health services MBS items 10950–10970
This document details how eligible patients should be billed for MBS items 10950 to 10970, including referral requirements, resources and access. -
Pharmaceutical Services Federal Committee of Inquiry
The Pharmaceutical Services Federal Committee of Inquiry (the Committee) was established by the Minister to address concerns that some instances of claiming contravened the National Health Act 1953. -
Pharmaceutical Benefits Scheme Non-compliance Fraud flyer
Information and advice for providers about Medicare compliance. -

Record keeping – quality improvement guide
This improvement guide is meant to help healthcare practitioners improve the quality of their record keeping. -
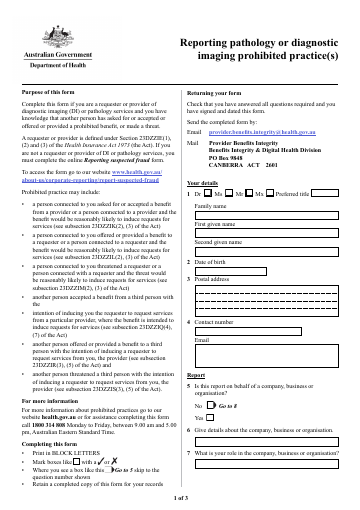
Reporting pathology or diagnostic imaging prohibited practices
Use this form if you are a requester or provider of diagnostic imaging (DI) or pathology services and want to let us know about another person who has asked for or accepted or
offered or provided a prohibited benefit, or made a threat. -
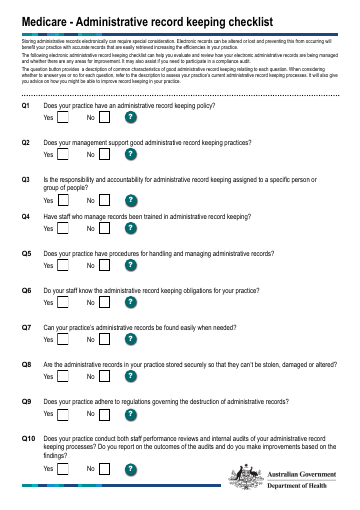
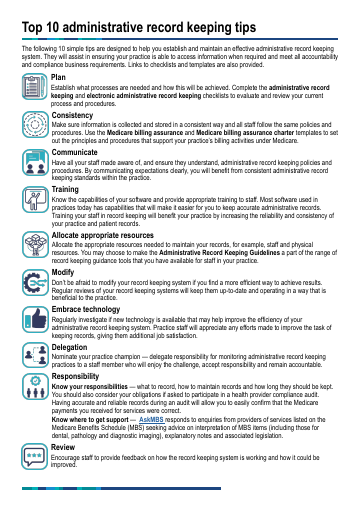
Medicare - Administrative record keeping checklist
The following checklist can help you evaluate and review how your electronic administrative records are being managed and whether there are any areas for improvement. It may also assist if you need to participate in a compliance audit. -
Practitioner review – a guide for those who employ or engage practitioners
Under the Health Insurance Act 1973 (Health Insurance Act), a person (including a practitioner) engages in inappropriate practice if they knowingly, recklessly or negligently cause or permit a practitioner who they employ or otherwise engage to engage in inappropriate practice. -

Frequently asked questions about Medicare billing in public hospitals
These FAQs answer commonly asked questions on public hospital funding for public patients, and appropriate Medicare billing for private patients in public hospitals. -
AskMBS Advisory – Allied health services – Part A Chronic disease management
AskMBS answers questions from health professionals about the Medicare Benefits Schedule -
Compliance Audit - Exceptional Circumstances Statutory Declaration
Use this form to provide details about any circumstances which prevent you from substantiating claimed Medicare or Child Dental Benefits Schedule (CDBS) services. -
Medicare provider numbers for dental hygienists, dental therapists, and oral health therapists
From 1 July 2022, dental hygienists, dental therapists, and oral health therapists can access Medicare provider numbers to directly claim for services under the Child Dental Benefits Schedule (CDBS). -
Nudge vs Superbugs: 12 months on
This is an update report to Nudge vs Superbugs: A behavioural economics trial to reduce the
overprescribing of antibiotics (Australian Government 2018). -
Final clinical committee report for Pain Management
This report contains the recommendations the Pain Management Clinical Committee made to the MBS Review Taskforce, after public consultation. -
Guideline for substantiating that a valid referral existed (from pathology or diagnostic imaging)
This guideline outlines what you can do to substantiate a service to be requested by another medical practitioner for Medicare Benefits Schedule (MBS) items 57521 and 65070. -
Guideline for substantiating that a valid referral existed (from specialist or consultant physician)
This guideline outlines what you can do to substantiate Medicare Benefits Schedule (MBS) items 104, 105, 110, 116, 122, 132, 133, 135, 141, 143, 145 and 147 that require receipt of a valid referral before the service is provided. -
Nudge vs Superbugs
A report into a behavioural economics trial to reduce the overprescribing of antibiotics. -
Administrative record keeping guidelines for health professionals
The Administrative Record Keeping Guidelines provides useful information and tools that support good administrative record keeping within your practice. -
Guideline for substantiating Ears, Nose and Throat Surgical Services
This guideline outlines what you can do to substantiate valid general ears, nose and throat surgical services were provided such as Medicare Benefits Schedule (MBS) items 41846, 41764 and 30473. -
Medicare billing assurance toolkit
A toolkit of checklists, templates and suggestions to make it easier for you to manage risks that inadvertently cause incorrect billing under Medicare.